Advice for parents and caregivers: Scarlet Fever and invasive Group A strep
We know that recent media reports about Scarlet Fever and Strep A may have caused concern among parents.
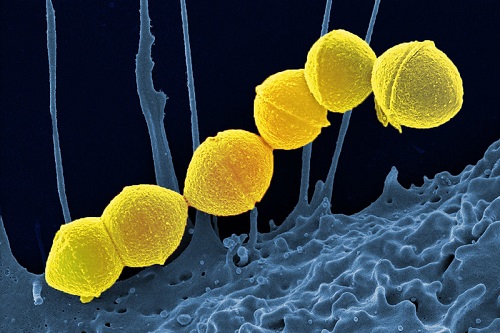
TV and radio news reports about Group A strep - a common bacteria which can cause a number of infections including Scarlet Fever - have caused some parents and carers to worry about their child's health, especially if they are currently unwell.
Scarlet fever
Scarlet fever is usually a mild illness, but it is highly infectious. So look out for symptoms in your child, which include a sore throat, headache, and fever, along with a fine, pinkish or red body rash with a sandpapery feel. On darker skin, the rash can be more difficult to detect visually but will have a sandpapery feel.



Photo credits: Don't forget the bubbles
Contact NHS 111 or your GP if you suspect your child has scarlet fever.
Early treatment of scarlet fever with antibiotics is important to reduce the risk of complications such as pneumonia or a bloodstream infection. If your child has scarlet fever, keep them at home until at least 24 hours after the start of antibiotic treatment to avoid spreading the infection to others.
Strep A and invasive Group A strep (iGAS)
Scarlet fever is caused by bacteria called group A streptococci. These bacteria also cause other respiratory and skin infections such as strep throat and impetigo.
In very rare occasions, the bacteria can get into the bloodstream and cause an illness called invasive Group A strep (iGAS). While still uncommon, there has been an increase in invasive Group A strep cases this year, particularly in children under 10.
Most children with GAS throat infection or Scarlet Fever will get better with antibiotics. Unfortunately, very occasionally some children become unwell later because their body produces an exaggerated immune response, or the bacteria gets into the blood stream and causes a more severe infection (called “invasive GAS” or iGAS).
Seeking help
As a parent, if you feel that your child seems seriously unwell, or is becoming more unwell even if they are on treatment or have recently finished antibiotics, you should trust your own judgement.
Contact NHS 111 or your GP if your child is getting worse despite paracetamol or ibuprofen if:
- the temperature has lasted more than 5 days
- your child is feeding or eating much less than normal, especially if they are drooling or appear in pain when swallowing
- your baby has had a dry nappy for 12 hours or more, or is crying without tears or your child shows other signs of dehydration:
- feeling thirsty
- dark yellow, strong-smelling pee
- peeing less often than usual
- feeling dizzy or lightheaded
- feeling tired
- a dry mouth, lips and tongue
- sunken eyes (dark circles under eyes)
- your baby is under 3 months and has a temperature of 38°C, or is older than 3 months and has a temperature of 39°C or higher
- your baby feels hotter than usual when you touch their back or chest, or feels sweaty
- your child is drowsy (much more sleepy than normal) or irritable (unable to settle them with cuddles, toys, TV or snacks – especially if they remain drowsy or irritable despite any fever coming down)
Call 999 or go to A&E if:
- your child is having difficulty breathing – you may notice grunting noises or their tummy sucking under their ribs or using their neck muscles to breathe
- there are long pauses (more than 10 seconds) when your child breathes
- your child’s skin, tongue or lips are blue
- your child feels very cold or clammy to touch
- your child is difficult to wake up or keep awake
- your child has severe pains in their arms, legs neck or back
- your child has a painful, red area of skin, especially if it is getting bigger quickly
Finding out more
Our NHS colleagues at the North Thames Paediatric Network have produced this patient information leaflet on scarlet fever - how to spot if your child may have it, what to do if you think they do and when to contact which NHS services.